The ultimate goal of clinical research is to provide relief from — and hopefully cures for — the various disorders that afflict human beings. In the ever-evolving world of research, effective regulation helps to ensure this ultimate goal remains dominant among the many motivations that drive research.
Institutional review boards (IRBs) are an important part of regulatory efforts. An IRB is an ethics review committee that is in place to ensure human research subjects’ rights are protected, as well as the rights of the patients who ultimately benefit from the research.
Operating under US federal regulations, state laws, and institutional policies, the IRB has the authority to approve, require modification to, and disapprove research. IRB approval is required for all human research.
An IRB review includes information about the physicians, scientists, and community members involved in the research.
Here’s a quick overview of IRBs and the expectations for working with them.
Who serves on an IRB?
A typical IRB is composed of physicians, a scientist, a non-scientist, and a representative from the community from which the human subjects are drawn.
Research trials sometimes involve the participation of human subjects who belong to what are considered “vulnerable populations”; i.e., children or incarcerated individuals who cannot adequately communicate their own interests with regard to informed consent. In such cases, federal regulations require that the IRB include a representative to protect the interests of those individuals.
Federal regulations (21 CFR 56,107e) prohibit the participation in an IRB of clinical investigators or others who may have conflicting interests.
Specific study responsibilities
Informed consent is a critical consideration for IRBs in their mission to insure protection of the rights and interests of the human subjects of research trials. The IRB is responsible for determining that informed consent forms provided to research subjects include all required information about the nature and extent of the activities involved in the research, and that the forms were reviewed and signed by the trial subjects.
The IRB further protects the interests of human subjects by reviewing the research trial in order to insure an appropriate balance of risks and benefits. Risk minimization efforts can include the use of already available data or processes. “There are safety provisions along the way,” explains Dr. Wanda Snead, research educator in the Global Quality and Education Department at Sarah Cannon Research Institute. “There’s monitoring of all of the aspects of the trial.” The IRB also is responsible for insuring that each step in the research trial process is properly documented and reported.
Equitable subject selection is also a critical IRB consideration. What is the rationale for the inclusion and exclusion criteria applied in subject selection? If vulnerable populations are to be involved, what is the justification? What measures are in place to protect the privacy and confidentiality of research subjects?
“The IRB will review all of this criteria,” says Dr. Snead, “and if they find any of it lacking, they can refuse the start of the trial until all of these matters are cleared.”
Does your research require IRB review?
- Is it research? U.S. Department of Health and Human Service Office for Human Research Protections (45 CFR 46) defines research as “a systematic investigation, including research development, testing and evaluation, [that] is designed to develop or contribute to the generalizable knowledge.” Based on this definition, case studies do not qualify as research because they are not systematic. Similarly, internal quality improvement activities do not qualify as research because they’re not designed to produce generalizable knowledge. In either case, IRB review is unnecessary.
- Does it involve human subjects? The involvement of human subjects in research is not limited to the use of the human body. Access to private information about the subject and the use of data or specimens also constitutes human involvement, as does interaction or intervention with the patient. Research “may not just be injecting the body with some new vaccine,” says Dr. Snead. “It could be just reviewing records or using data from the medical chart, and there may be blood samples or tissues samples that have been taken for perpetuity that can be linked back to an individual. Or it could be questionnaires or surveys and procedures.” Each of these examples involves a human subject, and as such is considered human research.
What an IRB wants to know
In fulfilling its oversight mission, an IRB seeks answers to certain key questions. Those answers provide the IRB with proof that the investigators and medical and scientific professionals involved in a study fully understand the ethical and technical requirements and standards that must be met in conducting the research.
The information the IRB is looking for includes:
- A clear definition and explanation of the activities, procedures, and protocols involved in the research;
- Specific information on the composition of the subject population and the inclusion/exclusion criteria used in the selection of human subjects;
- Proof of informed consent — the voluntary participation of human subjects; and
- Documentation of the risks and benefits of the proposed research.
“Investigators can’t just decide that they’re going to run a clinical trial,” explains Dr. Snead. “They’ve got to go through training in the rules and regulations, making sure that they can conduct the trial from an ethical standpoint.”
The IRB’s role is that of a watchdog, guarding the interests of the human subjects of the trial.
NIH policy mandates use of a single IRB (sIRB). And in January of this year, OHRP “Common Rule” regulations expanded the requirement to all federal research.
As a result, research sites will increasingly need to work with multiple IRBs, not just the local IRB. This impacts many aspects of how research sites conduct research and interact with the IRB, especially for sites previously accustomed to working with only a local IRB.
You may also like: What Goes Into An Instigator Site Fie
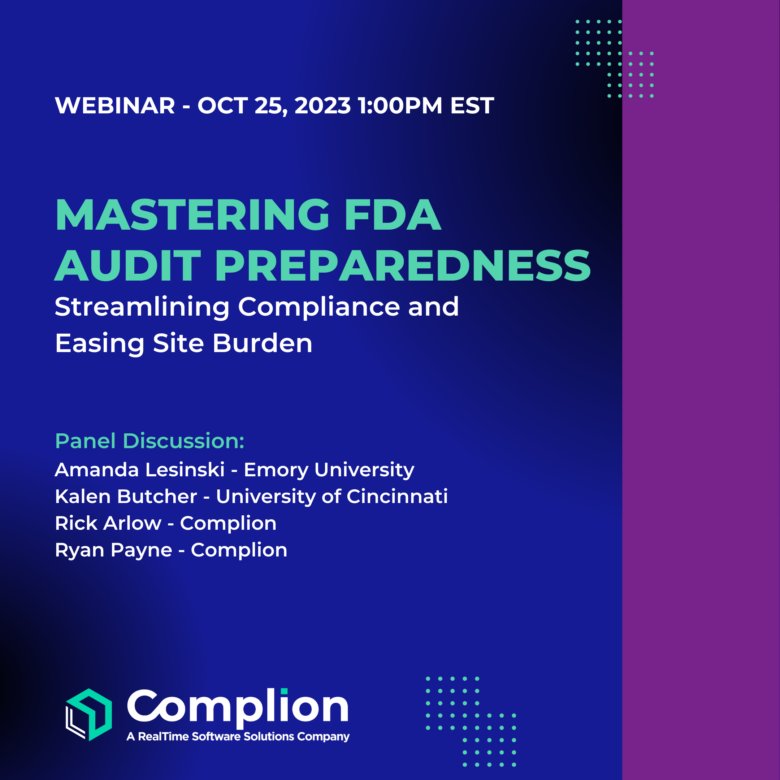
The Complion platform provides easy-to-use tools to file, control, share and central access all regulatory documents. Schedule a demo to learn more today.